Key Takeaways
-
Medicare Advantage plans often look ideal on paper, but their real-world performance can vary significantly based on network restrictions, prior authorizations, and regional availability.
-
The Centers for Medicare & Medicaid Services (CMS) issues star ratings, but a high score does not always guarantee that a plan will suit your specific healthcare needs or financial priorities.
The Promises of Medicare Advantage Plans
Medicare Advantage (Part C) plans are designed to offer a bundled alternative to Original Medicare. On paper, these plans seem to promise extensive benefits:
-
All-in-one coverage that includes Medicare Part A and Part B
-
Often includes Part D (prescription drug coverage)
-
Extra services such as dental, vision, hearing, fitness programs, and transportation
-
Annual out-of-pocket spending limits for Medicare-covered services
These features appeal to many retirees looking for predictable costs and added perks. But once you move beyond the brochure, the experience may not be as seamless.
CMS Star Ratings: A Standardized Measure, But Not a Guarantee
Each year, CMS assigns star ratings to Medicare Advantage plans. These range from 1 to 5 stars, with 5 being excellent. The ratings are based on factors such as:
-
Customer service
-
Chronic condition management
-
Member experience
-
Preventive care
-
Drug safety and pricing accuracy (for plans with Part D)
While a high star rating might indicate overall satisfaction and plan reliability, it doesn’t mean the plan will be ideal for your specific medical providers, prescriptions, or service area. It’s entirely possible for a 5-star plan to be poorly suited to your individual health priorities.
Real-World Use Brings Critical Trade-Offs
You might sign up for a Medicare Advantage plan expecting smooth coordination of care and strong value. But actual use can reveal several complications:
Limited Provider Networks
Most Medicare Advantage plans use a network of doctors, hospitals, and specialists. If your preferred providers are out-of-network:
-
You may face higher costs
-
You might not be covered at all unless it’s an emergency
-
Referrals may be required for specialist visits
This is especially problematic in rural areas, where fewer in-network providers may be available.
Prior Authorization Delays
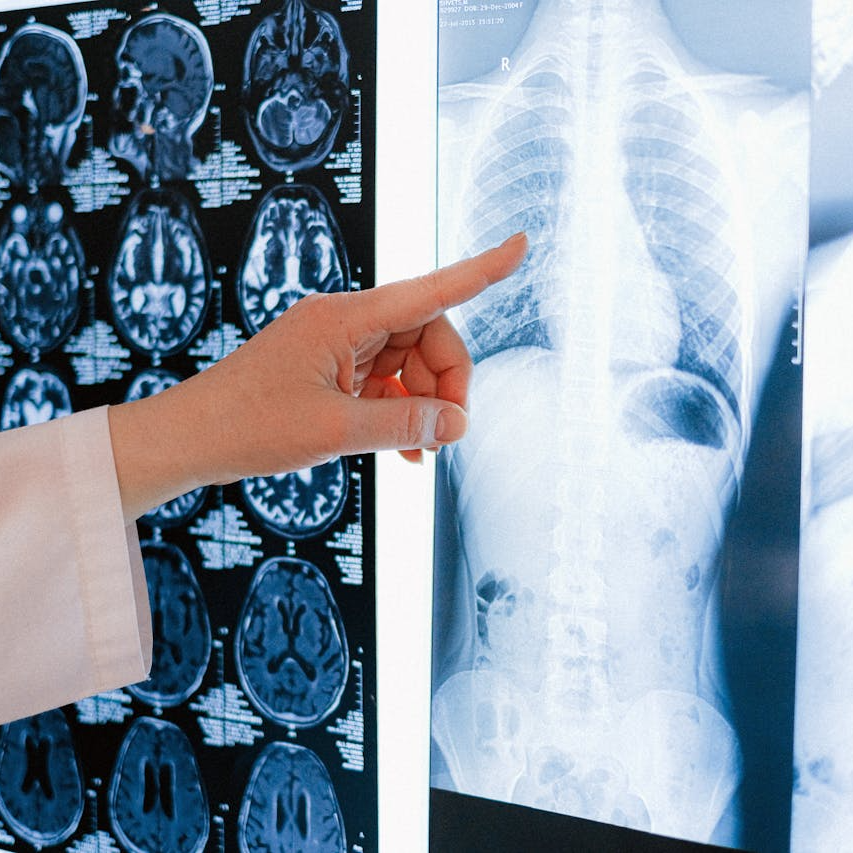
In 2025, prior authorization remains a major source of delays. Many Advantage plans require advance approval before covering:
-
Hospital stays
-
Outpatient surgeries
-
Imaging services (MRI, CT scans)
This requirement can lead to treatment delays or even denials if the paperwork isn’t completed correctly or reviewed promptly. According to CMS data, a significant share of these denials are later overturned, indicating inconsistencies in the initial decisions.
Coverage Gaps and Copayments
While Advantage plans must cover the same services as Original Medicare, they often structure cost-sharing differently:
-
You may pay copayments for each primary care or specialist visit
-
Hospital stays can involve daily copayments up to a certain number of days
-
Emergency room visits may carry a flat copay that is not waived even if you are admitted
Costs can add up quickly depending on how often you need care, especially if your plan has high copays for outpatient services.
Additional Benefits: Valuable or Just Eye-Catching?
Many Advantage plans advertise extra benefits, including:
-
Vision and dental care
-
Telehealth access
-
Over-the-counter allowances
These are certainly attractive, but they vary widely in quality and scope. For instance:
-
Dental coverage may include only cleanings and exams but not major services like crowns or dentures
-
Fitness memberships might be limited to select locations or specific types of programs
-
Over-the-counter allowances can be difficult to use if the selection is limited or ordering is complicated
In practice, these extras may offer limited financial value if they don’t align with your actual needs.
Rural vs. Urban Differences
Where you live affects your Medicare Advantage experience more than you might expect. In urban areas, you may have:
-
Multiple plans to choose from
-
Broad provider networks
-
Greater access to specialists
But in rural regions, plan options can be sparse. You might have to choose between:
-
A plan with few local providers
-
Traveling long distances to in-network care
Even high-rated plans struggle to serve rural populations effectively. The CMS star rating does not reflect geographic limitations, so you need to dig into each plan’s network details before enrolling.
Drug Coverage Under Part D: What’s Included?
Most Medicare Advantage plans include prescription drug coverage (MAPD plans). However, formulary design matters. Key concerns include:
-
Tiered drug pricing (generic vs. brand vs. specialty)
-
Step therapy requirements
-
Quantity limits
Some medications may not be covered or may require a trial of a lower-cost alternative first. This can be frustrating for individuals managing chronic conditions that require stable drug regimens.
In 2025, the Medicare Part D out-of-pocket maximum is $2,000. This cap offers important protection, but it only applies if the drug is actually covered under your plan’s formulary.
Plan Changes from Year to Year
Medicare Advantage plans are renewed annually, and your coverage in 2025 may look different from what you had in 2024. Common changes include:
-
Provider network changes (some doctors may leave the plan)
-
Increases in copayments or coinsurance
-
Changes to drug formularies or coverage rules
-
New rules for prior authorization
These updates are disclosed in the Annual Notice of Change, typically sent out each September. It’s essential to review this document carefully and consider switching plans during the Medicare Open Enrollment period (October 15 to December 7) if your current plan no longer meets your needs.
How to Evaluate a Medicare Advantage Plan in 2025
When reviewing your options, use a layered approach:
-
Start with Star Ratings: Use the CMS rating system as a broad quality indicator.
-
Check the Provider Network: Confirm that your preferred doctors and hospitals are in-network.
-
Review the Formulary: Ensure your prescriptions are covered and evaluate tier placement.
-
Compare Out-of-Pocket Costs: Examine maximum limits, copayments, and cost-sharing rules.
-
Understand Extra Benefits: Consider whether the extras will actually save you money or meet your needs.
-
Account for Travel Needs: If you spend time in different states or areas, look for plans with nationwide networks or travel coverage.
-
Anticipate Usage: Consider how often you expect to visit providers or specialists, and how those costs will add up over time.
Be Mindful of Marketing Language
Plans that rank as “best” in advertisements often do so based on limited criteria, such as premiums or availability of perks. These promotions may not reflect:
-
Regional differences in plan performance
-
Member complaints or disenrollments
-
How prior authorization impacts access
-
Service quality for chronic condition management
It’s critical not to make decisions based on headlines or commercials. Always use objective data from CMS and compare it against your personal needs.
What Works on Paper Doesn’t Always Work in Life
Medicare Advantage plans are complex. While they may provide important coverage and cost-saving opportunities, their success depends on alignment with your health priorities, location, provider access, and prescription needs.
Don’t assume that a plan that looks great on paper will perform just as well when it’s time to use it.
If you’re unsure about how a plan stacks up to your real-world needs, speak with a licensed agent listed on this website. They can help you compare plans, decode CMS star ratings, and explore coverage details that aren’t always visible in brochures.