Key Takeaways:
- Understanding what qualifies you for Medicare goes beyond just age; it includes your work history, certain medical conditions, and specific timelines.
- Enrolling at the right time helps you avoid penalties and ensures that your coverage starts when you need it most.
Medicare Basics: More Than Just Turning 65
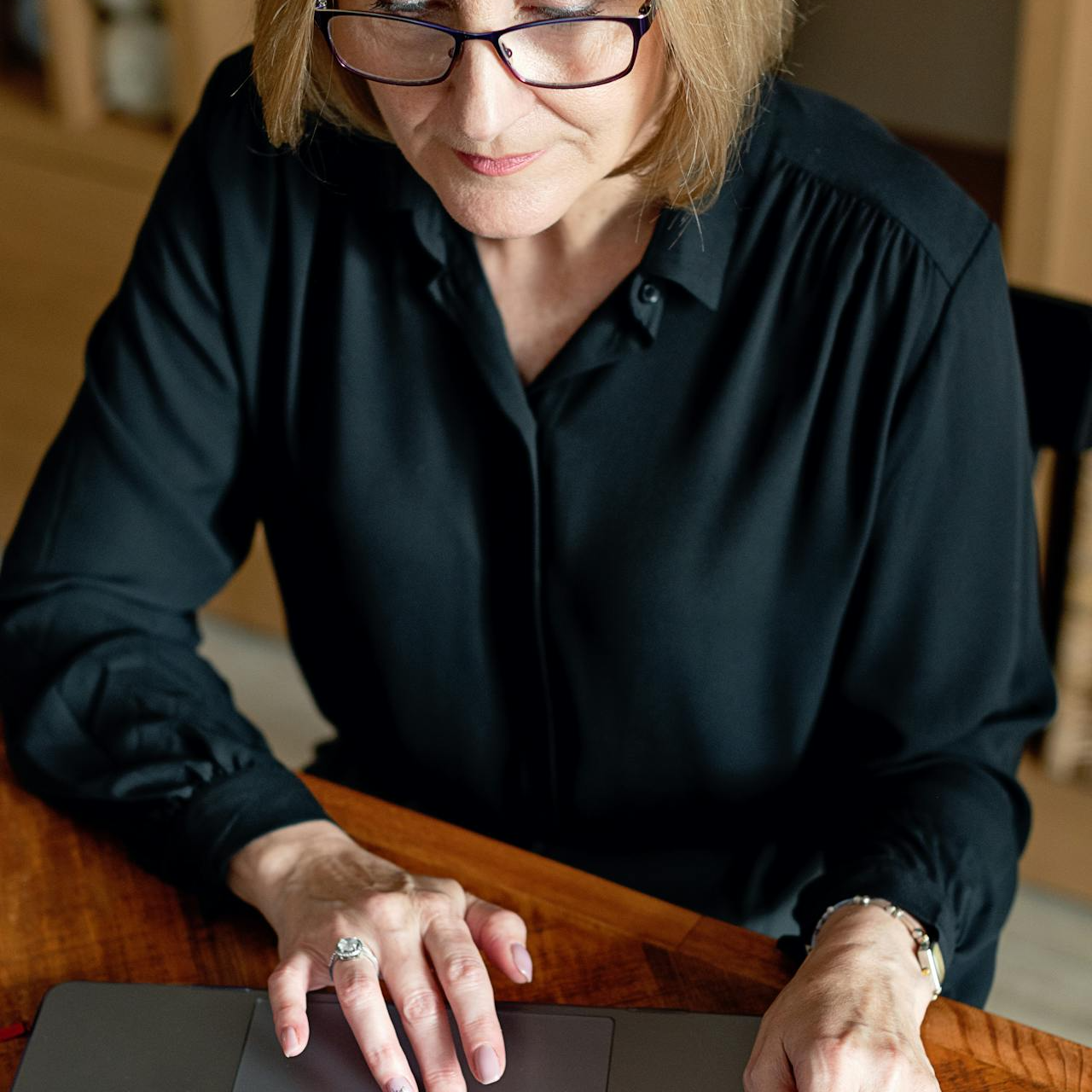
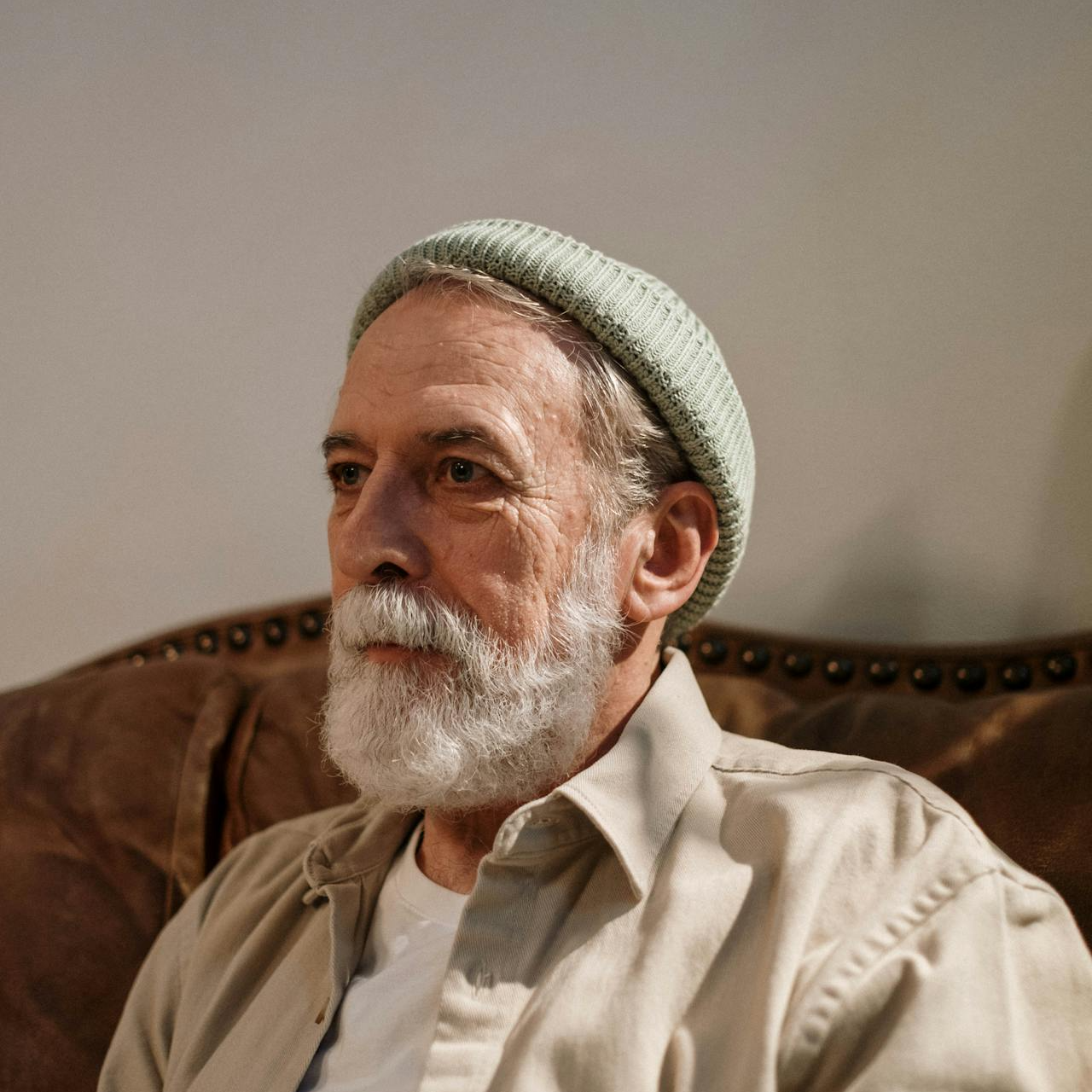
If you’re approaching Medicare age, you probably have questions about what makes you eligible and how to get started. The good news? You’re not alone, and I’m here to help demystify the process. While age is an essential part of qualifying for Medicare, there are other factors like work history and health conditions that play a significant role in determining your eligibility. Let’s break down everything you need to know so you can enroll with confidence.
Age 65: Your Starting Point
Turning 65 is a big deal for Medicare, and here’s why. For most people, it marks the beginning of their Initial Enrollment Period (IEP). This window lasts for seven months—three months before your 65th birthday, the month of your birthday, and three months after. Enrolling during this time is critical because it allows you to start your coverage without penalties or delays.
Why enroll on time? If you miss your IEP and don’t qualify for a Special Enrollment Period (SEP), you could face late enrollment penalties. For instance, the penalty for late Part B enrollment increases your premium by 10% for every 12-month period you delay.
Work History and Premium-Free Part A
Age might get your foot in the door, but work history can determine whether you qualify for premium-free Part A (hospital insurance). To receive Part A without a monthly premium, you or your spouse need to have worked and paid Medicare taxes for at least 40 quarters, which equals about 10 years.
Not enough work credits? Don’t worry—you can still enroll in Part A, but you’ll have to pay a monthly premium. If you have between 30 and 39 work quarters, you’ll pay a reduced premium, but it won’t be zero. The fewer your work quarters, the higher your premium, so knowing where you stand ahead of time helps you plan your finances.
Medicare Before 65: It’s Possible
Most people think of Medicare as something that starts at 65, but there are exceptions:
- Disabilities: If you’ve been receiving Social Security Disability Insurance (SSDI) for at least 24 months, you automatically qualify for Medicare. Your Medicare enrollment will begin in the 25th month of receiving SSDI benefits.
- ALS (Lou Gehrig’s Disease): If you’re diagnosed with ALS, you don’t have to wait 24 months. Medicare starts as soon as your SSDI benefits begin.
- End-Stage Renal Disease (ESRD): If you have ESRD and require dialysis or a kidney transplant, you can qualify for Medicare at any age. Coverage usually begins in the fourth month of dialysis treatment unless you meet specific criteria that allow earlier coverage.
The Role of Your Spouse’s Work History
Don’t have enough work credits to qualify for premium-free Part A? Your spouse’s work history could be your golden ticket. If your spouse has the required 40 quarters, you may qualify for premium-free Part A under their record. This also applies to divorced spouses as long as the marriage lasted for at least 10 years.
Widowed and divorced individuals: If you’re widowed or divorced but were married for 10 years or more, you might still be able to qualify based on your spouse’s work history.
Enrolling in Part B: Why Timing Matters
Part B (medical insurance) covers outpatient care, doctor visits, and other medical services. Everyone has to pay a premium for Part B, and unlike Part A, work history doesn’t change that.
Delaying Part B? If you choose to delay enrolling in Part B and don’t have other creditable coverage (like employer-provided insurance), be prepared for penalties. The penalty is 10% for each 12-month period you could have had Part B but didn’t enroll. This penalty lasts as long as you have Part B, which could mean higher costs for life.
Special Enrollment Periods (SEPs): A Safety Net
Still working at 65? If you have health coverage through your job or your spouse’s job, you might qualify for a Special Enrollment Period. This means you won’t face late enrollment penalties when you do sign up for Part B after your IEP ends. The SEP lasts for eight months after your employer coverage ends, giving you a buffer to transition to Medicare without added costs.
Important note: COBRA and retiree health coverage don’t count as active employment coverage, so don’t assume these will qualify you for an SEP.
General Enrollment Period (GEP): Last Resort
If you missed both your IEP and SEP, the General Enrollment Period (GEP) is your backup. It runs from January 1 to March 31 every year, with coverage starting on July 1. However, enrolling during this period may come with late penalties, so it’s best to avoid this situation if possible.
Medicare Part D: Don’t Forget Prescription Coverage
Part D, which covers prescription drugs, is another part of Medicare that you should think about when you become eligible. Even if you don’t take medications now, it’s wise to consider enrolling when you first become eligible to avoid future penalties. If you don’t sign up for Part D when you’re first eligible and go without creditable drug coverage for 63 consecutive days or more, you could face a late enrollment penalty. This penalty is calculated as 1% of the national base beneficiary premium times the number of months you went without coverage.
What About Medicaid and Dual Eligibility?
If you have limited income and resources, you may qualify for dual eligibility, meaning you’re eligible for both Medicare and Medicaid. This can help cover some or all of your out-of-pocket costs, including premiums, copayments, and deductibles. Medicaid rules vary by state, so it’s crucial to check your state’s guidelines to see if you qualify.
Tips for a Smooth Enrollment Process
So, how do you get started with Medicare? Here are some straightforward tips:
- Know your IEP timeline: Mark your calendar and set reminders so you enroll during your seven-month Initial Enrollment Period.
- Review your work history: Check your Social Security statement to ensure you have the necessary 40 quarters for premium-free Part A.
- Evaluate other coverage: If you’re still working or have other health insurance, compare it with Medicare to decide what works best for you.
- Get informed on Part D: Even if you don’t need it now, understanding your options can save you from late enrollment penalties later on.
- Ask questions: Don’t be afraid to reach out to Social Security or a Medicare counselor to get clarity on your specific situation.
Late Penalties: What You Need to Know
One of the most common pitfalls when enrolling in Medicare is misunderstanding the rules around late penalties. Here’s what you should keep in mind:
- Part B Penalty: For each 12-month period you delay, your premium goes up by 10%. This penalty sticks with you as long as you’re enrolled in Part B.
- Part D Penalty: The penalty for not enrolling in Part D when you’re first eligible is 1% of the national base beneficiary premium multiplied by the number of months you were without coverage. This penalty is also permanent.
Avoid these penalties by understanding your eligibility and enrolling when you’re supposed to.
Wrapping Up Your Medicare Journey
Medicare eligibility can feel complicated, but understanding the essentials—like age, work history, and special conditions—can make it much easier. Whether you’re getting ready to turn 65 or are exploring early eligibility due to a disability, knowing the rules will help you make informed decisions. Take time to review your work history, check your eligibility timelines, and plan your enrollment to get started on the right foot.
Understanding Eligibility and Getting Started with Medicare
Knowing what makes you eligible for Medicare and how to enroll at the right time can save you from penalties and ensure you get the coverage you need. With a clear understanding of the rules, you’ll be better prepared to navigate your path to Medicare.